Long COVID Drives Most Workers’ Comp COVID Costs in California
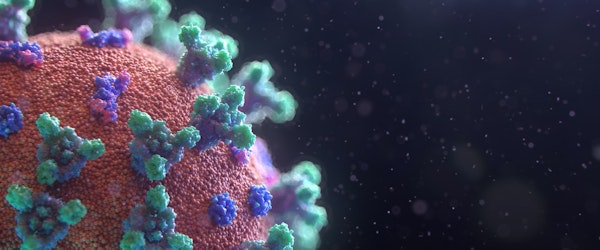
Wednesday, June 4th, 2025 Insurance Industry Life & Health Risk Management Workers' CompensationLong COVID continues to have a disproportionate financial impact on California’s workers’ compensation system, according to a recent study from the California Workers’ Compensation Institute (CWCI). Although only 4.7% of COVID-related claims from 2020 to 2022 involved Long COVID, these claims accounted for 73.7% of total costs and 82.1% of medical payments. The study examined over 126,000 insured and self-insured claims, revealing the outsized burden posed by prolonged recovery and ongoing health complications.
While the majority of COVID-related claims were minor—with just 14.6% involving any medical treatment—Long COVID claims were significantly more expensive. On average, medical payments for Long COVID cases were 105 times higher than for short-duration claims, while indemnity payments were 37 times greater. These long-tail claims typically involved extended time off work and persistent medical issues across various bodily systems.
The most common diagnostic categories for Long COVID included respiratory, circulatory, and nervous system conditions, with additional impacts observed in musculoskeletal, endocrine, mental health, and digestive systems. As California sees a drop in new COVID claims, concerns about vaccine access and future case surges may influence comp trends moving forward.
The CWCI report is available to members via the institute’s website, while non-members can purchase access. The findings underscore the long-term cost implications of pandemic-related claims on the workers’ comp system in the nation’s most populous state.




